 The gall bladder is another useful but expendable organ (see recent posts on the appendix and the spleen). Unlike losing your spleen, living without a gall bladder is not detrimental to your health, though it may be inconvenient at times.
The gall bladder is another useful but expendable organ (see recent posts on the appendix and the spleen). Unlike losing your spleen, living without a gall bladder is not detrimental to your health, though it may be inconvenient at times.
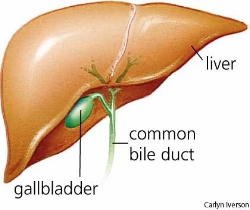
The gall bladder is located under the liver, on the right side of the body. It’s a small sac, about three inches long and 1 ½ inches wide when it’s full. It can hold a little under two ounces of bile (less than a quarter of a cup).
Bile is produced in the liver and stored in the gall bladder until it’s needed to digest fats. Fats need to be broken down (emulsified) before they can used by the body. When they’re not broken down, they pass right through the digestive track. That’s what can be inconvenient about not having a gall bladder. If you eat foods rich in fats, you may need to stay close to a restroom.
To visualize the emulsification of fat, think of a greasy frying pan in the sink. Rinsing with water does very little. But if you add detergent, the grease or fat (technically, a lipid) breaks down and can be rinsed away.
(This is the same thing that happens when you brush your teeth and then find that orange juice tastes terrible. The detergent in toothpaste breaks down the lipid membrane on the tongue. See Orange juice and toothpaste.)
Living without a gall bladder
A small muscular valve, called the sphincter of Oddi, controls the flow of bile (and pancreatic juices) to the intestines. When this sphincter is closed, bile flows into the gall bladder and not the intestines. Bile accumulates in the gall bladder between meals and becomes quite concentrated – up to five times more potent than the bile that exits the liver. When the digestive system needs bile, it secretes a hormone that causes the sphincter of Oddi to relax, and – voila – you’re ready to digest fats.
When you no longer have a gall bladder, your liver still makes bile, and there’s still a pathway (the common bile duct in the diagram) for bile to reach your digestive tract. The advantage of a gall bladder is that it contracts and squirts its contents into the small intestine just when you need it most: When you’re eating fat. In a previous post I described how the digestive system starts preparing for fat as soon as fat touches the tongue.
Without a gall bladder, bile flows continuously to the intestines, but it may not be potent enough to digest all the fat in a high fat meal. The effect would be similar to eating Olestra, the fat substitute Procter and Gamble briefly added to potato chips in the late 1990s. Olestra advertised itself as not adding fat, calories, or cholesterol to the potato chips. That was true because you couldn’t digest it. The FDA required a label on the packaging that said “Olestra may cause abdominal cramping and loose stools.” The condition was popularly known as “anal leakage.” Undigested fat – whether from Olestra or not enough bile – moves through the intestines more rapidly than you’d like.
Gallstones
The potent bile in the gall bladder can concentrate itself into little crystals. They’re made from cholesterol and calcium salts. Almost everyone has these gallstones, and they’re not necessarily a problem. One of the insurance industry cases I discussed a while back involved Otto Raddatz. He had received a CT scan that showed gallstones. His doctor never mentioned them because they were of no significance. He found out about them when his insurance company used them as the reason to cancel his insurance policy.
If gallstones are as small as a grain of sand, they’ll pass effortlessly through the bile ducts that lead to the small intestines. If they’re the size of golf balls, that’s much too big. There will be pain and the risk of infection.
There’s no absolutely certain way to prevent gallstones. One thing that’s definitely not good is fasting. What keeps the gall bladder healthy are regular meals that include some fat. It stands to reason that if the contents of the gall bladder aren’t emptied regularly, there’s more opportunity for gallstones to grow. You want to keep your bile flowing. (See The Spleen in Chinese Medicine for some ancient advice on regular eating habits.)
How to increase health care costs: Unnecessary gall bladder removals
In a recent post on The Health Care Blog, Dr. Bob Wachter tells a story about his experience with patients undergoing gall bladder surgery. When Dr. Wachter was a medical student in the 1980s, surgeons removed the gall bladder only when it was infected (or if the patient was diabetic). Patients with gall stones were told to avoid fatty foods and to get immediate attention if they had severe pain and a fever. Most people with gallstones died with their gall bladders intact.
In the late 1980s, surgeons developed a procedure to remove the gall bladder laparoscopically – through a small incision using a video camera. Previously a gall bladder operation was an “up to the elbows” procedure. It required a week in the hospital, a month’s recuperation, and produced a large scar. The surgery was painful, had a high rate of complications, and the number of deaths following surgery was non-trivial. It was also expensive.
The advent of laparoscopic surgery changed all this. The hospital stay was much shorter. Convalescence was faster. Complications were lower. Hardly anyone died. And it cost 25% less. Sounds good, right? But consider what happened.
Gall bladder surgery was now regarded as so harmless that doctors began to recommend it to anyone who had “symptomatic gallstone disease,” that is, anyone with gallstones and abdominal pain. What with the increased use of CT scans and ultra sounds, more people were found to have (harmless) gallstones. And who doesn’t get a belly ache now and then? So a lot of people qualified for the operation.
In medicine this is called “indication creep.” Increasingly less significant risk indicators become a reason to remove the gall bladder. Another example of indication creep is the increasingly lower levels of serum cholesterol that trigger the prescription of statins. Indication creep is related to the increasing medicalization of previously normal conditions (pregnancy, menopause, ED).
The “Fats Are Unhealthy” fiasco
In 1977 the US Senate Select Committee on Health and Human Needs held hearings on the relationship between diet and chronic disease. One of the recommendations that came out of those hearings was to reduce the amount of fat in the American diet, even though there was limited knowledge at the time about what constituted a health-promoting diet.
For the next twenty years, reducing fat consumption was a primary goal of the US government and nutritionists. And what happened? We had an enormous increase in obesity and diabetes, which we’re still trying to explain. One suggestion is that fat reduction led to increased carbohydrate consumption.
Given the timing of the “indication creep” for gall bladder surgery – it started in the 1980s – I wonder if there’s any correlation with the promotion of a low fat diet? If health conscious individuals eliminated fat from their diets, that could have led to an increase in the size of gallstones. I can remember avoiding fat like the plague in those days. There were reports that fat consumption was related to breast cancer.
This is a pure speculation. Even if there was a correlation, that says nothing about cause and effect.
The operation
Here’s a short and sweet video of a laparoscopic cholecystectomy (gall bladder removal), narrated in a voice designed to produce hypnotic anesthesia.
Related posts:
Do we taste fat?
Why do we love high-fat foods?
Orange juice and toothpaste
Why health insurance isn’t there when you need it most
How the pharmas make us sick
Still useful after all these years: The appendix
Still useful after all these years: The spleen
The Spleen in Chinese Medicine
Collateral circulation and the cat concerto
Sources:
(Links will open in a separate window or tab.)
Bob Wachter, Explaining Runaway Costs: The Lobster or the Salad?, The Health Care Blog


Sorry, comments are closed for this post.