In a perfect world, doctors would not prescribe – and patients would not take – drugs that do more harm than good. But it’s complicated. The benefits and harms of drugs are determined in randomized, controlled clinical trials. For many reasons, the outcomes of such trials may not provide doctors with the information they need to decide who should take what.
In a perfect world, doctors would not prescribe – and patients would not take – drugs that do more harm than good. But it’s complicated. The benefits and harms of drugs are determined in randomized, controlled clinical trials. For many reasons, the outcomes of such trials may not provide doctors with the information they need to decide who should take what.
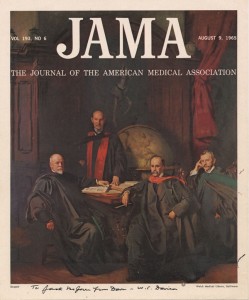
For example, harmful effects (like death) may not show up during the limited time span of a trial. Data from trials may be selected – and other data ignored — to produce positive results. This is apt to happen when clinical trials are conducted by the pharmaceutical industry, rather than by economically disinterested parties, such as the NIH or independent academic institutions. Also, the participants in the trial may differ significantly (in age, gender, and health, e.g.) from patients who end up taking the drugs. As a recent article in JAMA put it, “most clinical trials fail to provide the evidence needed to inform medical decision making.”
The Inverse Benefit Law
If you follow pharma news, you will have noticed that many high profile, aggressively marketed drugs turn out to be either ineffective or positively dangerous (think Vioxx, widely prescribed for arthritis, which turned out to cause heart attacks and stroke). Howard Brody, MD, and Donald Light, PhD, have proposed an explanation for this phenomenon. They call it the Inverse Benefit Law: “The ratio of benefits to harms among patients taking new drugs tends to vary inversely with how extensively the drugs are marketed.” Or (for those who feel fuzzy about inversion): The more aggressively a drug is marketed, the more likely the drug will cause harm, be ineffective, or deliver little by way of benefit. Read more